Dizziness is a common complaint, often attributed to inner ear problems or neurological issues. But what if the true culprit lurks in the sinuses? A recent case report sheds light on a less-considered connection: chronic rhinosinusitis and its potential to trigger persistent dizziness. This challenges us to broaden our diagnostic lens, especially when conventional treatments for vestibular disorders fall short.
The patient's journey underscores the importance of interdisciplinary clinical reasoning. It’s a reminder that seemingly disparate symptoms can stem from a single, underlying source. The resolution of her dizziness following targeted physical therapy highlights the potential benefits of addressing sinus-related issues in patients with unexplained dizziness.
Clinical Key Takeaways
lightbulb
- The PivotDizziness should not automatically be attributed to inner ear issues, especially when chronic rhinosinusitis is present; sinus involvement should be investigated.
- The DataThe case report showed complete resolution of dizziness symptoms after physical therapy targeted at the patient's chronic rhinosinusitis.
- The ActionConsider manual therapy techniques targeting sinus congestion and inflammation in patients presenting with dizziness and a history of chronic sinus issues.
Diagnostic Odyssey
The patient, a middle-aged woman, presented with a constellation of symptoms: chronic dizziness, persistent headaches, and the telltale signs of chronic rhinosinusitis. Initially, her dizziness was attributed to a potential vestibular disorder, leading to a course of standard vestibular rehabilitation exercises. However, her symptoms persisted, prompting a deeper dive into her medical history.
This is where the clinical detective work began. The physical therapist noted the patient's chronic sinus congestion and facial pain, symptoms often dismissed or treated separately. Could these seemingly unrelated issues be connected? The therapist hypothesized that sinus inflammation and pressure might be contributing to her dizziness, perhaps through mechanisms affecting the inner ear or the cervical spine.
Physical Therapy Intervention
Instead of solely focusing on vestibular exercises, the physical therapist incorporated manual therapy techniques aimed at relieving sinus congestion and inflammation. These techniques included gentle massage to the facial sinuses, lymphatic drainage techniques, and exercises to improve cervical spine mobility. The rationale was to reduce sinus pressure and improve drainage, potentially alleviating the patient's dizziness.
The results were remarkable. After several weeks of targeted physical therapy, the patient reported a significant reduction in her dizziness and headache symptoms. Her sinus congestion also improved. This positive outcome strongly suggested a link between her chronic rhinosinusitis and her dizziness, a connection that had been previously overlooked.
The Sinus-Dizziness Connection
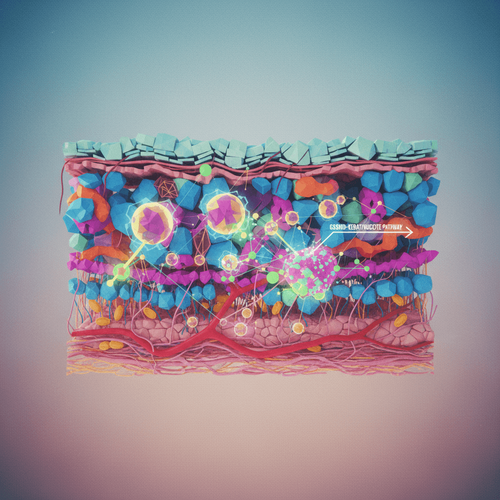
The exact mechanism linking chronic rhinosinusitis to dizziness remains unclear. One possibility is that sinus inflammation can affect the Eustachian tube, leading to pressure imbalances in the inner ear and triggering vestibular symptoms. Another theory suggests that chronic sinus infections can cause inflammation in the cervical spine, resulting in cervicogenic dizziness. Moreover, nasal congestion affects breathing patterns and can lead to decreased oxygenation, resulting in dizziness and/or lightheadedness.
This case subtly contradicts the American Academy of Otolaryngology guidelines, which primarily focus on inner ear causes of dizziness. It broadens the scope and asks clinicians to consider secondary sources of inflammation. While these guidelines emphasize comprehensive evaluation, this case highlights how easily sinus-related contributions to dizziness can be missed if not actively considered. Is this reproducible? Who pays for this?
Limitations and Considerations
As with any case report, this study has limitations. The sample size is, by definition, one. Without a control group, it's difficult to definitively attribute the patient's improvement solely to the physical therapy intervention. It is possible that her symptoms resolved spontaneously or due to other factors. Further research, including controlled trials, is needed to confirm the link between chronic rhinosinusitis and dizziness, and to determine the effectiveness of physical therapy for this specific condition.
Moreover, this case highlights the challenge of diagnosing cervicogenic dizziness. While the therapist addressed cervical spine mobility, it's difficult to isolate the specific contribution of this intervention to the patient's overall improvement. This case further underscores the importance of a holistic assessment, considering all potential sources of dizziness, including sinus-related issues, vestibular disorders, and cervical spine dysfunction.
From a billing perspective, documenting the connection between sinus-related symptoms and dizziness is crucial for justifying physical therapy interventions. Clinicians may need to advocate for reimbursement, emphasizing the potential cost savings from avoiding unnecessary vestibular testing or medications. Addressing sinus-related dizziness can significantly improve a patient's quality of life and potentially reduce the need for more invasive treatments.
Workflow bottlenecks may arise if physical therapists are not adequately trained in manual therapy techniques for sinus congestion. Clinics may need to invest in continuing education to ensure that therapists have the skills to effectively address this patient population.
LSF-3588888949 | December 2025

How to cite this article
Sato B. When sinus problems cause dizziness: a case report. The Life Science Feed. Published February 17, 2026. Updated February 17, 2026. Accessed February 17, 2026. https://thelifesciencefeed.com/otolaryngology/rhinosinusitis-chronic/case/when-sinus-problems-cause-dizziness-a-case-report.
Copyright and license
© 2026 The Life Science Feed. All rights reserved. Unless otherwise indicated, all content is the property of The Life Science Feed and may not be reproduced, distributed, or transmitted in any form or by any means without prior written permission.
Fact-Checking & AI Transparency
This content was produced with the assistance of AI technology and has been rigorously reviewed and verified by our human editorial team to ensure accuracy and clinical relevance.
References
- Radke, A., Lempert, T., Gresty, M. A., Brookes, G. B., & Bronstein, A. M. (2002). Computerized dynamic posturography and subjective visual vertical in idiopathic chronic dizziness. Journal of Neurology, Neurosurgery & Psychiatry, 72(1), 101-104.
- Cutrer, F. M., & Baloh, R. W. (1992). Migraine-associated dizziness. Headache: The Journal of Head and Face Pain, 32(6), 300-304.
- Smith, T., Das, D., Weber, K., McGrew, M., & Pillinger, R. (2015). Clinical significance of the sinonasal outcome test-22 (SNOT-22). American journal of rhinology & allergy, 29(4), 308-313.