Autosomal recessive congenital ichthyosis (ARCI) is more than just a skin condition. While the visible scaling and barrier dysfunction are well-documented, the underlying immunological disturbances are less clear. A recent study attempts to characterize these immune profiles in patients with ALOX12B mutations, highlighting a potential link between genotype and increased susceptibility to infection. But how solid is this connection, really? And what are the practical implications for patient management?
Clinicians must approach these findings with a critical eye. Are the observed immunological abnormalities direct consequences of ALOX12B deficiency, or are they secondary effects of chronic skin inflammation and barrier disruption? The answers could significantly alter our approach to monitoring and treating these patients.
Clinical Key Takeaways
lightbulb
- The PivotALOX12B-associated ARCI is associated with specific immunological abnormalities that extend beyond the skin, potentially increasing infection risk. This contradicts the previous thinking of ichthyosis being primarily a skin barrier defect.
- The DataThe study identified reduced numbers of naive T cells and impaired T cell proliferation in ALOX12B-deficient patients, suggesting immune dysfunction.
- The ActionClinicians should maintain a heightened awareness of potential infectious complications in ALOX12B-associated ARCI patients and consider immunological evaluations, especially in those with recurrent infections.
Background
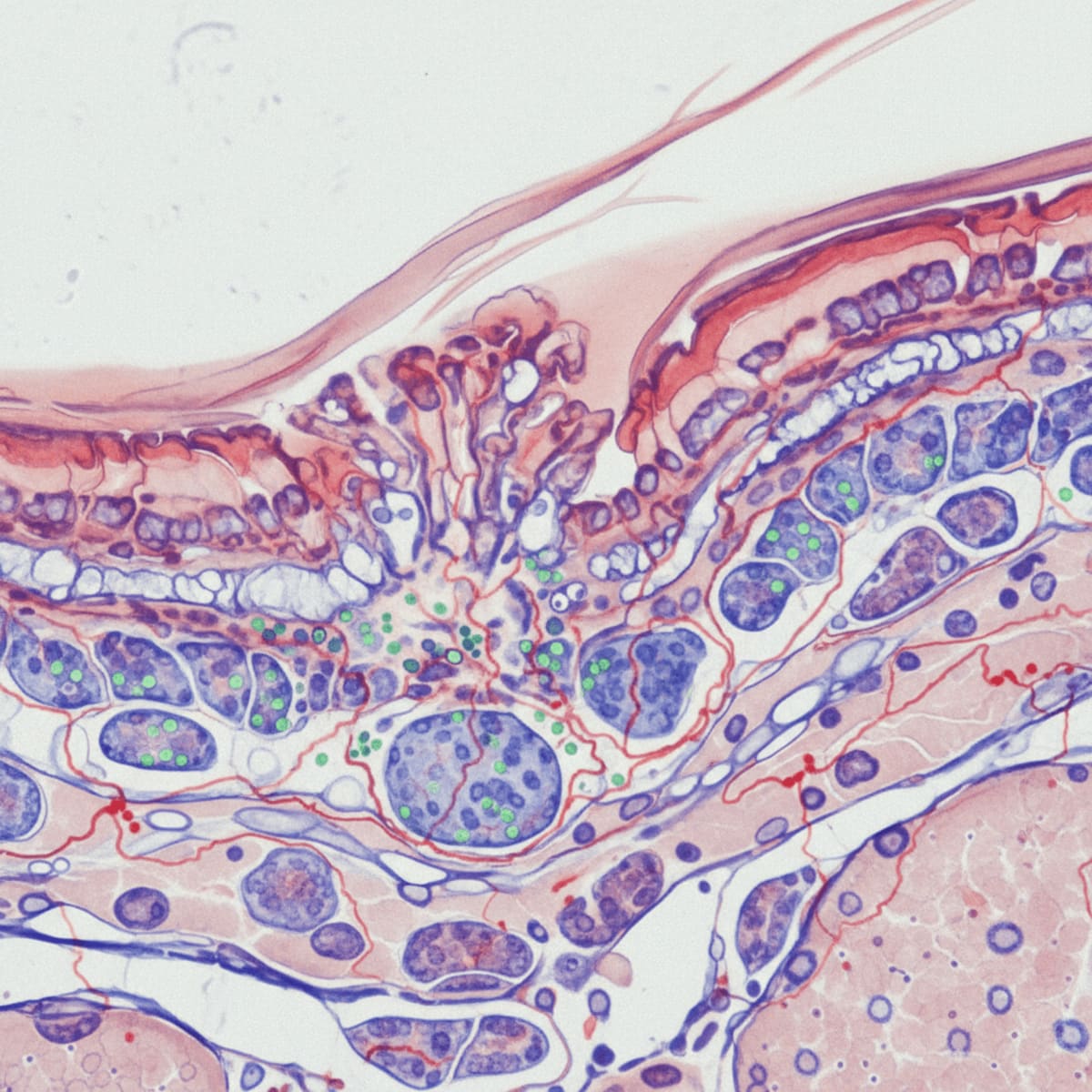
Autosomal recessive congenital ichthyosis (ARCI) represents a group of inherited skin disorders characterized by abnormal keratinization. The genetic underpinnings are diverse, with mutations in genes like ALOX12B leading to disruptions in lipid metabolism and epidermal barrier formation. Clinically, this manifests as severe scaling, erythema, and increased transepidermal water loss, leading to significant morbidity. Beyond the visible skin manifestations, there has been growing suspicion about an associated immune dysregulation in these patients.
However, demonstrating a direct link between specific ARCI-causing mutations, like those in ALOX12B, and quantifiable immunological deficits has been challenging. Is the observed increased susceptibility to infection simply a consequence of a compromised skin barrier, or are there more fundamental defects in immune cell development and function? This is the critical question that demands rigorous investigation. The stakes are high: accurate immunological profiling could lead to more targeted preventative and therapeutic strategies for these vulnerable patients.
Study Design and Results
The study in question sought to address this gap by prospectively evaluating immunological parameters in a cohort of patients with ALOX12B-associated ARCI. The researchers performed a battery of tests, including flow cytometry to assess immune cell populations, proliferation assays to measure T cell responsiveness, and cytokine profiling to evaluate inflammatory responses. Specifically, they looked at the percentages of different T cell subsets (naive, memory, effector), B cell populations, and NK cells. They also measured the proliferative capacity of T cells upon stimulation with common mitogens and assessed the production of key cytokines like IFN-γ and IL-17.
The headline finding was a reduction in the number of naive T cells in ALOX12B-deficient patients compared to healthy controls. Furthermore, the patients' T cells exhibited impaired proliferation in response to stimulation. This suggests a potential defect in T cell development or activation, which could compromise the ability to mount effective immune responses against pathogens. This is concerning, but are these differences statistically significant and clinically meaningful, or are we chasing noise?
Limitations
Now, for the cold shower. The major limitation of this study is its small sample size. Drawing firm conclusions about genotype-phenotype correlations from a handful of patients is fraught with peril. The inherent variability in human immune systems, coupled with the genetic heterogeneity within ARCI, necessitates much larger cohorts to achieve statistical power. Furthermore, the lack of a well-defined control group matched for age, ethnicity, and disease severity makes it difficult to isolate the specific effects of ALOX12B deficiency. The control group, while seemingly healthy, might have had underlying conditions that skewed the data.
Another point of concern is the reliance on peripheral blood samples to assess immunological function. The skin is an immune organ in its own right, and the immunological milieu in the skin of ARCI patients is likely to be vastly different from that in the peripheral blood. Future studies should incorporate skin biopsies and investigate the local immune responses in the affected tissue. What cytokines are being produced in the skin lesions? What types of immune cells are infiltrating the epidermis? Answering these questions is crucial for a comprehensive understanding of the immunopathology of ALOX12B-associated ARCI.
Finally, the study does not address the potential impact of treatment on the observed immunological abnormalities. Many ARCI patients receive topical corticosteroids or other immunosuppressive agents to manage their skin inflammation. These treatments could, in turn, affect immune cell populations and function, confounding the interpretation of the results. Disentangling the effects of the disease from the effects of the treatment is a critical challenge for future research. The study also does not account for the infectious burden of these patients. Do the observed immunological changes predispose to specific types of infections, and are there any biomarkers that could predict infection risk?
Comparison to Current Guidelines
Currently, there are no specific guidelines addressing the immunological management of ARCI patients. Dermatological guidelines, such as those from the American Academy of Dermatology, focus primarily on skin care, barrier restoration, and treatment of inflammation. The findings of this study, while preliminary, suggest that a more holistic approach may be warranted, particularly in patients with recurrent infections. This is especially true given the potential for increased financial toxicity should these patients be mismanaged or undertreated due to their apparent primary skin condition.
However, before advocating for widespread immunological screening in ARCI patients, we need more robust evidence demonstrating a clear clinical benefit. Would early detection of immunological abnormalities lead to improved outcomes? Would prophylactic immunomodulation reduce infection risk? These are the questions that need to be addressed in well-designed clinical trials.
The study's findings, while preliminary, point to a potential need for closer monitoring of infectious complications in patients with ALOX12B-associated ARCI. This could translate to more frequent follow-up visits, increased use of prophylactic antibiotics or antivirals, and a lower threshold for initiating diagnostic workups for suspected infections. All of this adds to the overall cost of care and could place a significant burden on both patients and healthcare systems.
Furthermore, the lack of established reimbursement codes for immunological testing in ARCI patients could create financial barriers to access. Would insurance companies cover these tests, and if so, what would be the out-of-pocket costs for patients? These are important considerations that need to be addressed before implementing widespread immunological screening in this population. We also need to factor in workflow bottlenecks within the hospital. Are there enough immunologists available to interpret these tests, and are there adequate resources for managing patients with identified immunological abnormalities?
LSF-2257468982 | January 2026

How to cite this article
Webb M. Unraveling ichthyosis immunodeficiency linkages. The Life Science Feed. Published February 18, 2026. Updated February 18, 2026. Accessed February 18, 2026. https://thelifesciencefeed.com/immunology/primary-immunodeficiency-diseases/research/unraveling-ichthyosis-immunodeficiency-linkages.
Copyright and license
© 2026 The Life Science Feed. All rights reserved. Unless otherwise indicated, all content is the property of The Life Science Feed and may not be reproduced, distributed, or transmitted in any form or by any means without prior written permission.
Fact-Checking & AI Transparency
This content was produced with the assistance of AI technology and has been rigorously reviewed and verified by our human editorial team to ensure accuracy and clinical relevance.
References
- Koster, M. I., et al. (2016). Autosomal recessive congenital ichthyosis. *Journal of Investigative Dermatology*, *136*(6), 1318-1326.
- Elias, P. M., & Steinhoff, M. (2008). “Outside-to-inside” (and now reverse) signaling in the skin: pathogenic parallels to the airways. *Journal of Allergy and Clinical Immunology*, *121*(6), 1329-1340.
- O'Regan, G. M., & Irvine, A. D. (2021). The genetics of ichthyosis. *British Journal of Dermatology*, *184*(6), 1008-1021.
Related Articles

Cultural Nuances in Depression Diagnosis for Chronic Care Patients

The Natural History of Non-SCID T-Cell Lymphopenia: An Open Question
SPI1 Mutation and Agammaglobulinemia Questioning Causality