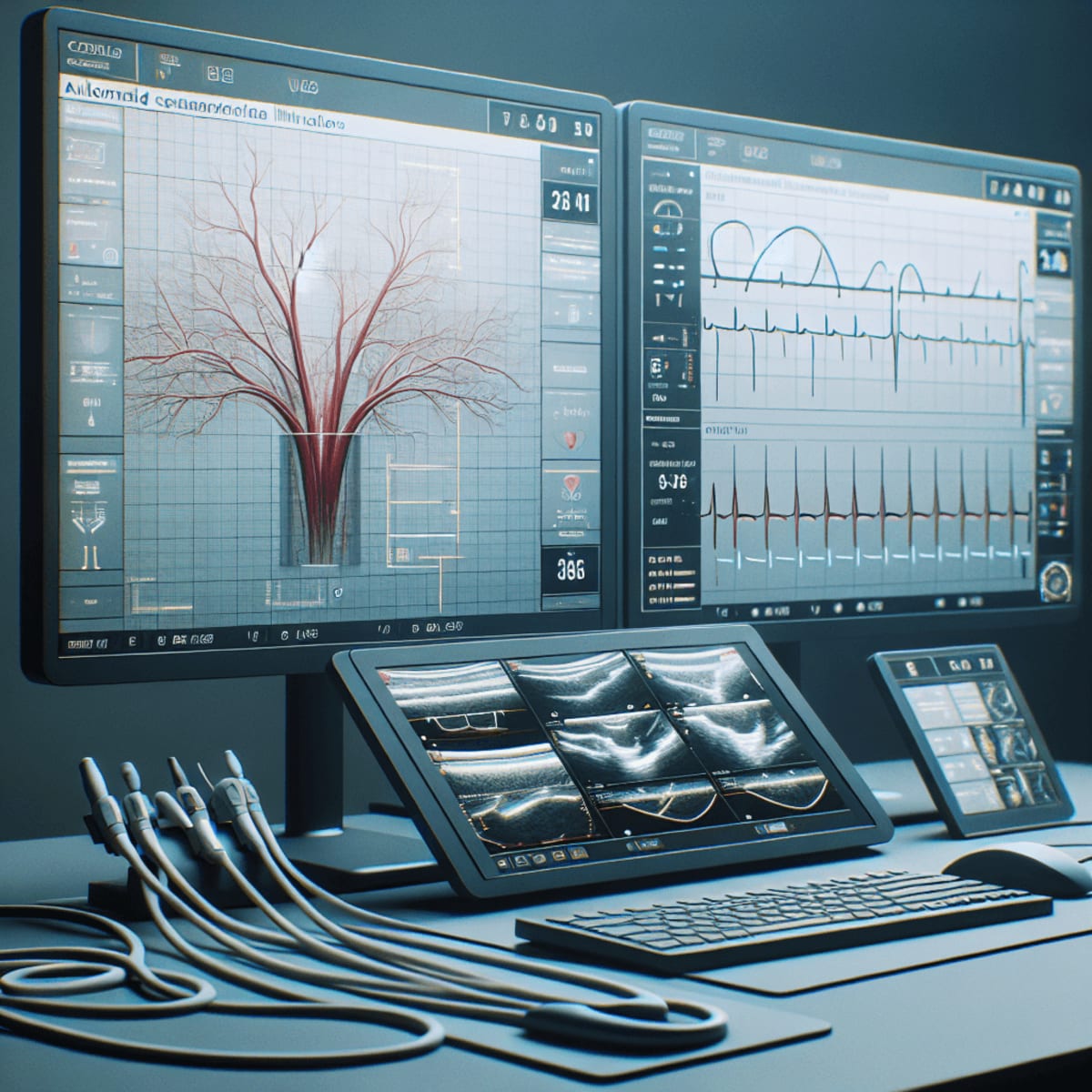
Coronary artery anomalies complicate decision-making because morphology and course can be nuanced, dynamic, and variably documented across imaging modalities. Intravascular ultrasound offers cross-sectional visualization that can clarify lumen size, vessel remodeling, and wall pathology, yet manual tracing remains time-intensive and operator-dependent. AIVUS-CAA reports an automated approach to IVUS image processing and quantification tailored to anomalous coronary anatomy, aiming to standardize how lumen, vessel wall, and related metrics are derived.
This article examines where automation can reduce variability, how segmentation and measurement pipelines might be organized, and what validation and governance are needed for clinical adoption. We outline potential clinical use cases, interoperability considerations, and research opportunities that could position automated quantification as a practical bridge between imaging and procedural planning.
Why automate IVUS for coronary artery anomalies
Reliable quantification is foundational when evaluating anomalous coronary anatomy and its hemodynamic implications. Many patients with an anomaly also have or are at risk for Coronary Artery Disease, making standardized assessment of plaque, vessel size, and luminal geometry clinically relevant. IVUS can complement angiography when anatomy is tortuous, when ostial takeoff is uncertain, or when interarterial or intramural segments are suspected. Automating measurements in this setting targets a bottleneck where manual planimetry can be inconsistent, especially when image quality varies or when calcification and shadowing complicate interpretation.
Consequences of non-standardized reporting include fragmented baselines, limited comparability between centers, and challenges in procedural planning for stenting or surgical reimplantation. An automated pipeline can align measurements with best-practice conventions, such as consistent frame selection, edge detection rules, and reporting formats. The goal is not to replace expert reading but to provide a reliable first pass that reduces cognitive load and flags frames that merit closer review. This approach can also cut time to decision in urgent settings while preserving traceability for governance and audit.
Clinical context and unmet needs
Although prevalence estimates of congenital anomalies vary, the clinical problem is less about rarity and more about measurement uncertainty. In this niche, the first value proposition is simply consistency: the same rules applied every time to derive lumen area, external elastic membrane surrogates, and segment length. A unified reporting template can also facilitate multidisciplinary discussions where surgeons and interventionalists require precise dimensions. By anchoring measurements to a standardized protocol, downstream risk stratification and procedural planning can be better aligned across teams.
Automation is especially compelling when IVUS is used to clarify ambiguous angiography or CT findings. Early, reproducible quantification enables longitudinal comparisons even when operators change or when imaging devices differ. For trainees, automated overlays can orient attention to key landmarks while demonstrating how decisions derive from measurements. In quality programs, they allow systematic review of outliers and errors to improve training, acquisition technique, and device selection.
From qualitative impressions to quantitative baselines
Clinicians typically start with visual impressions of lumen shape, eccentricity, and wall features. Translating these impressions into numbers requires reliable edge finding and noise handling. Automated quantification makes those steps explicit and repeatable, allowing users to track how measurements change across pullbacks. When the same pipeline is applied to follow-up scans, a true baseline emerges, improving confidence in interval change assessments.
Inside AIVUS-CAA: pipeline, measurements, and QC
The AIVUS-CAA concept centers on automated segmentation of IVUS frames and consistent derivation of lumen and vessel metrics. IVUS physics introduces acoustic artifacts, ring-down noise, and shadowing, making robust segmentation non-trivial. Algorithms must work across catheters, pullback speeds, and consoles while accommodating real-world imaging variability. The reported software focuses on automation tuned to anomalies, where ostial and proximal segments, and transitions across intramural portions, can challenge standard assumptions.
Data ingestion and preprocessing
Successful automation begins with standardized data ingestion. A well-designed pipeline will ingest DICOM or vendor-native formats and normalize frame rates, pullback speeds, and gray-scale distributions. Preprocessing steps typically include ring-down correction, despeckling, and contrast normalization to stabilize edge detection. This scaffolding creates a predictable frame-by-frame environment where downstream models can perform consistently across studies and sites.
Preprocessing also encodes metadata relevant to interpretation, such as catheter position, pullback direction, and frame spacing, enabling faithful conversion of pixel-level measurements into millimeter-scale metrics. When these steps are deterministic and logged, users can reproduce results and audit any deviations from the default pipeline. That traceability is crucial for clinical governance and for multi-institutional research.
Segmentation models and the lumen-vessel interface
Automating contouring hinges on robust Image Segmentation, the technical core of mapping intensity patterns to anatomical boundaries. In IVUS, the lumen-intima interface and the media-adventitia boundary can be obscured by calcium, stent struts, or shadowing. A data-driven approach may combine classical filters with contemporary Machine Learning models optimized for edge continuity and artifact tolerance. Beyond static per-frame contours, longitudinal smoothing across consecutive frames can enforce physiological plausibility and reduce frame-to-frame jitter.
Because anomalies often include ostial involvement, the pipeline must handle eccentric shapes and abrupt changes in vessel size or course. A hybrid strategy that blends geometric priors with learned features can stabilize segmentation where acoustic artifacts are common. The output includes lumen area and a vessel surrogate that can be used to estimate plaque burden, with confidence measures to guide human review when the signal is weak. These design choices turn IVUS data into structured measurements suitable for aggregation and trend analysis.
Plaque metrics and anomaly descriptors
Quantitative descriptors enable clearer communication and comparison between cases. Metrics may include minimum lumen area, percent area stenosis, eccentricity indices, and curvature or tortuosity proxies relevant to anomalous courses. When feasible, automated estimates that support Plaque Characterization can contextualize stenosis severity, though calcium and shadowing remain limiting factors. For anomalies, descriptors that capture intramural segments, interarterial course, or slit-like ostia can be standardized to reduce ambiguity in reports.
A consistent dictionary of terms also supports Quantitative Imaging registries and multi-site studies, where reproducible definitions are essential. Summarizing findings in a structured table or synoptic report facilitates comparison with invasive physiology or cross-modality imaging. Importantly, outputs must flag uncertainty, encouraging expert readers to validate critical frames before clinical decisions are finalized.
Quality control and uncertainty
A credible system bakes in explicit quality control gates. Confidence heatmaps can highlight frames where the lumen border is uncertain or where the media-adventitia boundary is ambiguous. These flags enable readers to prioritize manual review where it is most impactful. Transparent uncertainty estimates are also essential to governance, supporting audits, second reads, and clinician trust.
An automation pipeline should document failure modes and provide user-visible reasons for fallback behavior. For instance, if ring artifacts force a conservative lumen estimate, the software should label that assumption. Such design makes the tool safer in edge cases and more teachable for new users. It also supports systematic improvement by aggregating failure examples for retraining.
Interoperability and workflow integration
Real-world utility depends on seamless integration with cath lab consoles and reporting systems. Exporting measurements and contours in standard formats facilitates Interoperability with PACS, registries, and research databases. Tight coupling to reporting tools can auto-populate fields, reducing transcription errors and manual calculation. Role-appropriate alerts can notify the operator when a minimum lumen area falls below a configurable threshold, prompting additional imaging or physiology.
From a process standpoint, automation should reduce, not add, steps in the workflow. Ideal deployments enable near-real-time overlays that support decisions during the same procedure. Offline batch processing can be useful for research and for longitudinal reviews where multiple timepoints are compared. Regardless of mode, results must be traceable to source frames to preserve clinical accountability.
Implications, validation, and next steps
AIVUS-CAA aligns with a broader shift toward reproducible, machine-assisted measurement in cardiovascular imaging. When measurements are consistent, multicenter collaboration becomes easier and benchmarking becomes meaningful. In anomalies, better quantification can inform the balance between surveillance and intervention. The reported approach emphasizes automation tuned to anomalous anatomy, where typical vessel assumptions may not hold and where robust error handling is vital.
Clinical use cases and decision support
Automated quantification can enhance pre-procedural planning by characterizing proximal dimensions and ostial morphology before stent sizing or surgical planning. It may also add value in follow-up, where consistent baselines underpin surveillance for restenosis or remodeling. When combined with physiology, quantitative IVUS can refine risk assessment by correlating anatomic severity with functional impact. These capabilities can mature into targeted Clinical Decision Support, provided that guardrails and explainability are maintained.
Benchmarking and regulatory pathway
For clinical adoption, external validation against expert tracings and prospective testing in diverse anomaly phenotypes are essential. Benchmarks should include intra- and interobserver variability, processing time, and failure rates in predefined edge cases. Comparative evaluations with existing semi-automated tools can clarify incremental value, especially if automation reduces time without sacrificing accuracy. Regulatory submissions will likely hinge on transparent performance claims, predefined indications for use, and a monitoring plan for post-market updates.
Equity, generalizability, and human factors
Generalizability depends on training data diversity across vendors, catheter types, and acquisition protocols. Sites with lower signal-to-noise or legacy hardware should still see reliable performance, or be informed when confidence drops. Human factors matter: overlays must be legible, defaults sensible, and user controls minimal but meaningful. Clear visual cues that differentiate automated contours from manual edits can reduce cognitive friction and maintain user trust.
What to watch in the next 12 months
Key signals to monitor include open validation cohorts, shared benchmarking datasets, and transparent performance dashboards. Integrations that auto-populate structured reports will test whether automation truly saves time in busy labs. Prospective registries can assess clinical impact, such as time-to-decision, rates of additional imaging, or concordance with invasive physiology. Users should also watch for governance features, including versioning, audit trails, and site-level calibration tools.
Initial details about AIVUS-CAA and its intended capabilities are available via the PubMed record for the software description: Automated Intravascular Ultrasound Image Processing And Quantification Of Coronary Artery Anomalies: The AIVUS-CAA Software. As with any new tool, strengths will be clarified by independent testing and real-world use. Expected benefits include time savings, reduced variability, and more transparent reporting. Ultimately, the value of automation will rest on durable improvements in consistency and communication across the heart team.
Looking ahead, a practical path is iterative: deploy in a controlled workflow, capture feedback, and refine. Success will depend on how well the system balances sensitivity with specificity, speed with traceability, and automation with clinician oversight. If these trade-offs are managed well, automated IVUS quantification could become routine in anomaly workups and a template for other specialized imaging tasks. The promise is credible because it targets a well-defined pain point and converts qualitative impressions into shareable, reproducible numbers.
LSF-8325115428 | November 2025
How to cite this article
Team E. Automated ivus quantification for coronary artery anomalies. The Life Science Feed. Published November 11, 2025. Updated November 11, 2025. Accessed January 31, 2026. .
Copyright and license
© 2026 The Life Science Feed. All rights reserved. Unless otherwise indicated, all content is the property of The Life Science Feed and may not be reproduced, distributed, or transmitted in any form or by any means without prior written permission.
Fact-Checking & AI Transparency
This summary was generated using advanced AI technology and reviewed by our editorial team for accuracy and clinical relevance.
References
- Automated intravascular ultrasound image processing and quantification of coronary artery anomalies: The AIVUS-CAA software. https://pubmed.ncbi.nlm.nih.gov/40972478/.